Why is this drug prescribed?
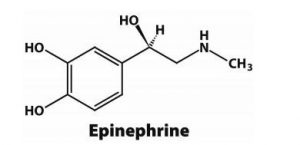
Epinephrine injection is used along with emergency medical treatment to treat life-threatening allergic reactions caused by insect stings or stings, foods, medications, latex, and other causes. Epinephrine is in a class of medications called alpha and beta-adrenergic agonists (sympathomimetic agents). It works by relaxing the muscles in the airways and tightening the blood vessels.
How should this medicine be used?
Epinephrine injection comes as a prefilled automatic injection device containing a solution (liquid) and in vials for injection subcutaneously (under the skin) or intramuscularly (into the muscle). It is usually injected as needed at the first sign of a severe allergic reaction. Use epinephrine injection exactly as directed; do not inject more often or inject more or less than prescribed by your doctor.
Ask your doctor or pharmacist to show you and any caregivers who may be injecting the medicine how to use the prefilled automatic injection device. Training devices are available to practice using the automatic injection device during an emergency. The training devices are drug-free and needle-free. Before you use epinephrine injection for the first time, read the patient information that comes with it. This information includes instructions on how to use the prefilled automatic injection device. Be sure to ask your pharmacist or doctor if you or your caregivers have any questions about injecting this medication.
You should inject epinephrine injection as soon as you suspect you may be experiencing a serious allergic reaction. Signs of a serious allergic reaction include the closing of the airways, wheezing, sneezing, hoarseness, hives, itching, swelling, redness of the skin, rapid heartbeat, weak pulse, anxiety, confusion, stomach pain, loss of control of urine or bowel movements, fainting, or loss of consciousness. Talk to your doctor about these symptoms and make sure you understand how to tell when you’re having a severe allergic reaction and need to inject epinephrine.
Keep your automatic injection device with you or available at all times so you can quickly inject epinephrine when an allergic reaction starts. Please note the expiration date stamped on the device and replace it when this date passes. Look at the solution on the device from time to time. If the solution is discoloured or contains particles, call your doctor for a new injection device.
Epinephrine injection helps treat severe allergic reactions, but it is not a substitute for medical treatment. Get emergency medical treatment immediately after injecting epinephrine. Rest easy while you await emergency medical treatment.
Most automatic injection devices contain enough solution for one dose of epinephrine. If your symptoms continue or return after the first injection, your doctor may direct you to use a second dose of epinephrine injection with a new injection device. Make sure you know how to inject the second dose and how to know if you need to inject a second dose. Only one health care provider should give more than 2 injections for a single allergic episode.
Epinephrine should be injected only in the middle of the outer thigh and can be injected through clothing if needed in an emergency. If you are injecting epinephrine into a young child who may move during the injection, hold their leg firmly in place and limit the child’s movement before and during the injection. Do not inject epinephrine into the buttocks or any other part of the body, such as the fingers, hands, or feet, or into a vein. Do not place your thumb, fingers, or hand over the needle area of the automatic injection device. If epinephrine is accidentally injected into these areas, get emergency medical treatment right away.
After injecting an injection dose of epinephrine, some solution will remain in the injection device. This is normal and does not mean that you have not received the full dose. Do not use the extra liquid; dispose of any remaining liquid and device properly. Take the user device to the emergency room or ask your doctor, pharmacist, or health care provider how to dispose of used injection devices safely.
Other uses of this medicine
This medication may be prescribed for other uses; ask your doctor or pharmacist for more information.
What secondary effects can this medication cause?
Epinephrine injection may cause side effects. When receiving emergency medical treatment after injecting epinephrine, tell your doctor if you experience any of these side effects:
- skin redness, swelling, warmth, or tenderness at the injection site
- labored breathing
- strong, fast, or irregular heartbeat
- nausea
- vomiting
- perspiration
- dizziness
- nervousness, anxiety, or restlessness
- soft spot
- pale skin
- headache
- uncontrollable shaking of a part of your body
What should I know about the storage and disposal of this medicine?
Keep this medication in the plastic tube it came in, tightly closed, and out of the reach of children. Keep it at room temperature and away from light, excess heat and moisture (not in the bathroom). Do not refrigerate epinephrine injection or leave it in your car, especially in hot or cold weather. If the prefilled automatic injection device is dropped, check for cracks or leaks. Throw away any medicine that is damaged or should not be used and make sure you have a replacement available.
Unnecessary medicines must be disposed of in a special way to ensure that pets, children and others cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medicine is through a medicine take-back program. Talk to your pharmacist or contact your local trash/recycling department to find out about take-back programs in your community.
It is important to keep all medicines out of the sight and reach of children, as many containers (such as weekly pill reminders and those for eye drops, creams, patches, and inhalers) are not child-resistant and small children can easily open them. To protect young children from poisoning, always close the safety caps and immediately put the medication in a safe place, one that is up high, away, and out of their sight and reach.
In case of emergency/overdose
- sudden weakness or numbness on one side of the body
- sudden trouble speaking
- slow or fast heart rate
- difficulty breathing
- fast breathing
- Confusion
- tired or weak
- cold and pale skin
- decreased urination

